Depression and anxiety are common paralleling symptoms in patients with Ulcerative Colitis (UC) and Inflammatory Bowel Disease (IBD) [1]. Often, the mental symptoms precede the physical symptoms in patients with UC by about a year [1]. The reverse is generally true of IBD, with depression or anxiety following the actual physical disease [1]. Whether the mental symptoms follow or precede the physical disease, the connection is shown in both clinical and research settings.
Depression and anxiety are common paralleling symptoms in patients with Ulcerative Colitis (UC) and Inflammatory Bowel Disease (IBD) [1]. Often, the mental symptoms precede the physical symptoms in patients with UC by about a year [1]. The reverse is generally true of IBD, with depression or anxiety following the actual physical disease [1]. Whether the mental symptoms follow or precede the physical disease, the connection is shown in both clinical and research settings.
There is a strong correlation between IBD and a microbial imbalance of the intestinal flora. Genetically modified animals, engineered to have IBD, but in a germ-free environment, didn’t develop colitis [9]. The connection between the gut and the brain, mainly through the vagus nerve, is a key player in mental and emotional health [7]. There is also a connection between depression and small intestinal bacterial overgrowth [10]. A healthy gut flora is essential for proper metabolism of complex lipids and polysaccharides, synthesis of vitamin K, pantothenic acid and folic acid, in improving intestinal motility and in protecting the digestive tract from pathogens, drugs and cancer causing agents [7,8]. A disruption in the gut flora’s sensitive balance between “good” and “bad” bacteria could easily lead to the malabsorption of these key nutrients needed for creation of neurotransmitters, the chemicals in our brain that regulate emotions. The ingestion of probiotics, even just from yogurt, has been shown to improve mood in patients with depression [8].
Several studies have shown a strong correlation between the consumption of junk food (high energy, low nutrition) and psychiatric distress and violence in adolescents [3]. It’s feasible to assume that by improving childhood nutrition, it may be possible to prevent later antisocial or aggressive behavior [3].
There seems to be a cycle of malnutrition leading to sadness and in turn, depressed mental state leading to even more malnourishment. For this reason, it is important to monitor and/or supplement any of the common nutrient deficiencies associated with both IBD and depression such as omega-3 fatty acids, folic acid, zinc, magnesium, Vitamin A, B6, B12, K and D [2,4,10].
Serotonin and cholecystokinin(CCK) are two neurotransmitters humans make, which are produced in the digestive tract, that help to regulate mood, amongst other things. Serotonin is commonly correlated to depression and other psychological disorders in modern day medicine. However, CCK is rarely implicated as a cause of mental health.
CCK stimulates the production of insulin, pancreatic enzymes and the contraction of the gallbladder which are all essential to a healthy gut. It also helps to modulate the release of dopamine, better known as our happy neurotransmitter [5]. Dysregulation of CCK has been correlated to melancholy, as well as to the early satiety and malabsorption of essential nutrients [5,6]. Damage to intestinal lining could cause a depletion in release of these necessary peptides. Supplementation can be given to increase serotonin, insulin and pancreatic enzymes, but to treat the root cause, the gut lining must be healed and restored to improve one’s own neurotransmitters.
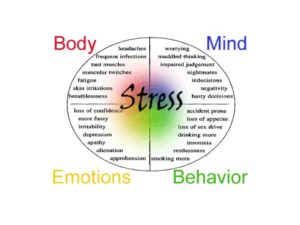
Stress is commonly linked to the cause or exacerbation of both UC, IBD, dysbiosis and depression [1,10]. Reduction of stress, whether it is from an internal or external source, is one of the first courses of actions towards restoring health [2]. Guided imagery has been used to decrease anxiety and stress in patients with IBD. This form of meditation helped to significantly reduce pain as well [11]. Melatonin, which is known as a sleep regulator and powerful antioxidant, also plays a role in the regulation of gastrointestinal motility and sensation. It has also been shown to relieve symptoms of IBS, including improvements in sleep, anxiety and depression [2].
Brain derived neurotrophic factor (BDNF) is essential to the functionality and survival of the nervous system [10]. This is often low in patients with Major Depressive Disorder (MDD) and the depletion of BDNF may be associated with depression-associated neuronal atrophy in the hippocampus and prefrontal cortex of the brain [10]. In both IBD and MDD, high levels of inflammatory chemicals are often seen. Along with removing any allergenic foods and a high fiber diet, probiotics can help to alter these inflammatory markers and may ultimately lead to an increase in BDNF, improving brain and nerve health [2,10].
Since the inception of naturopathic medicine, treating the gut has been a key component for treating many pathologies including mental health diseases. As this new wave of appreciation for naturopathic medicine comes to the forefront, we already see conventional medical doctors like Dr. Oz and Dr. Andrew Weil promoting this concept. Because of these doctors, there has been an ever growing amount of studies proving this connection and in doing so, proving the aphorism of ‘treating the gut’ which is essential to getting to the root cause of a disease and practicing the principles of naturopathic medicine.
Works Cited
- Kurina, L.M. & et.al. “Depression and anxiety in people with inflammatory bowel disease.” J Epidemiol Community Health Volume 55(2001):716-720
- Gaby, Alan R. Nutritional Medicine. Concord, NH: Fritz Perlberg Publishing, 2011. Print.
- Zahedi, H. & et.al. “Association between junk food consumption and mental health in a national sample of Iranian children and adolescents: The CASPIAN-IV study.” Nutrition Volume 30 Issue 11–12(2014): 1391–1397
- Vagianos, K. & et.at. “Nutrition Assessment of Patients With Inflammatory Bowel Disease” J Parenter Enteral Nutr Volume 31 No. 4(2007): 311-319
- “CHOLECYSTOKININ; CCK”. Online Mendelian Inheritance in Man. Johns Hopkins University, copyright 1966-2014. http://omim.org/entry/118440
- Geracioti T.D. Jr & et al. “Meal-related cholecystokinin secretion in eating and affective disorders.” Psychopharmacol Bull. Volume 25 Issue 3(1989):444-9.
- Gonzalez-Cervantes, R., Bravo-Ruiseco, G. & Pacheco-Lopez, G. ”The microbiota-gut-brain axis: neurobehavioral correlates, health and sociality.” Front Integr Neurosci. Volume 7 Issue 70(2013): web.
- Dinan, T.G. & Quigley E.M. “Probiotics in the treatment of depression: science or science fiction?” AUST NZ J PSYCHIATRY Volume 45 Issue 12(2011 Dec): 1023-5.
- Hiromasa, T. & et al. Imbalance in intestinal microflora constitution could be involved in the pathogenesis of inflammatory bowel disease. International Journal of Medical Microbiology Volume 298 Issues 5–6(1 July 2008):463–472
- Logan, A.C. & Katzman, M. Major depressive disorder: probiotics may be an adjuvant therapy. Medical Hypotheses Volume 64 Issue 3(2005): 533–538
- Mizrahia, M.C. & et al. Effects of guided imagery with relaxation training on anxiety and quality of life among patients with inflammatory bowel disease. Psychology & Health Volume 27 No. 12(December 2012): 1463–1479.